Bridging the ‘Death Gap’; and other Inequalities of US Healthcare
Published: July 13, 2022
As we develop novel medical devices here at Casana, one of our core design principles is inclusivity. Our focus on inclusivity stems from the need to address systematic disadvantages which are pervasive within the United States healthcare system. There are studied differences in the standard of care, and mortality rates, for minority groups and socio-economically disadvantaged populations in the US.
The Death Gap
The introduction of the ‘death gap’, otherwise known as the mortality gap, can be traced back to the 1973 book, Differential Mortality in the United States by Evelyn Kitagawa and Philip Hauser. Kitagawa & Hauser’s research is known for documenting lower mortality rates and longer life expectancy in those with higher income and education levels. Life expectancy is often used as a measure of the health of a country or a community when assessing the impact of socioeconomic inequalities.
Since 1973, it has become an increasingly accepted fact that socio-economic factors—including income, education, and occupation—can affect an individual’s lifespan on average. Dr. David Ansell, a Chicago-based physician, social epidemiologist, and author, has championed the discussion on the effects of social-structural factors on an individual’s health.
“There’s a 35-year difference in life expectancy between the healthiest and wealthiest and the poorest and sickest neighborhoods in America. For example, 30 blocks apart in New York City, the life expectancy of people in Harlem is 10 years less than those living on the Upper East Side; in Los Angeles, 16 years of life expectancy vanishes along a short stretch of the 405 highway.” – David A. Ansell, MD, MPH
The following case studies on Hypertension, Pulse Oximeters, and Gender/Race Representation in research studies are examples of how inequalities that impact healthcare are systemic to the US healthcare system.
Case Study: Social Vulnerabilities Negatively Impact Hypertension
Hypertension, otherwise known as high blood pressure, was a primary or contributing cause of death for 516,955 people in the United States in 2019 according to the CDC. Nearly half of adults in the United States (47%, or 116 million) have hypertension, which puts them at risk for both heart disease and stroke, the leading causes of death in the United States. Known as the silent killer, due to its asymptomatic nature, hypertension can only be diagnosed by having your blood pressure measured or monitored. This is usually done in a clinical setting, although recent advancements in remote patient monitoring have enabled a shift to home-based care.
The American Heart Association published a study comparing how social vulnerabilities (low income, less education, living in a poverty-stricken zip code, etc.) and health disparities (such as a lack of health insurance) are predictive of a hypertension diagnosis and ultimately, mortality. This AHA study utilized data from the REGARDS study (Reasons for Geographic and Racial Differences in Stroke) and included participants without baseline hypertension.
The researchers concluded that those with more vulnerabilities were more likely to develop hypertension and to have died in ten years, than those with no identified vulnerabilities. The study demonstrated that an individual’s count of social vulnerabilities (0, 1, or ≥2) can be used to identify high-risk adults and begin proactive care regimes (including remote patient monitoring) to delay or even prevent hypertensive incidents which might lead to death. Hypertension is one of the many health conditions that contributes to the death gap in America.
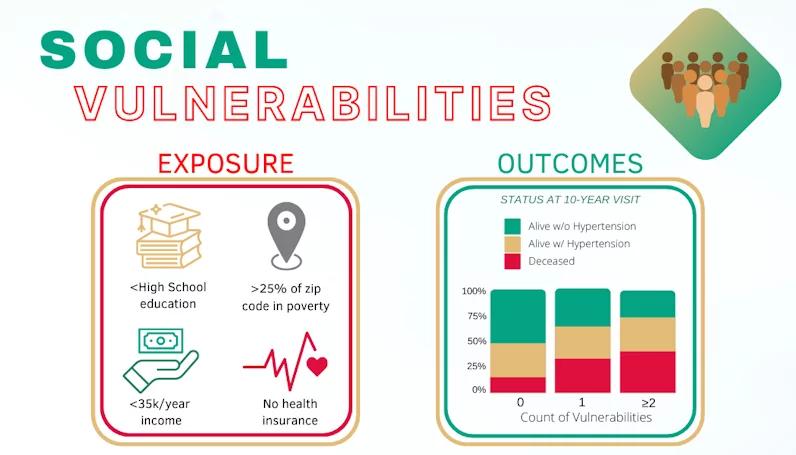
Data Sourced from, “Multiple Social Vulnerabilities to Health Disparities and Hypertension and Death in the REGARDS Study”.
There are many factors in the US healthcare system that disproportionately impact low-socioeconomic households. Going into a clinic for blood pressure measurements or even simply buying a blood pressure cuff, for example, can be considerably challenging for individuals due to factors such as low income, strenuous commutes (living in remote locations), as well as inflexible employment hours. The impact of socioeconomic factors on healthcare is extensive, but they are just one aspect that influences the care that patients may (or may not) receive.
Case Study: Pulse Oximeters Failing Dark Skin Tones
The advent of the COVID-19 pandemic has highlighted the importance of self-monitoring, especially in regard to blood oxygenation (which refers to the proportion of oxygen you have circulating in your blood). This is usually done by utilizing a pulse oximeter, but an increasing amount of attention in the US media has focused on the failure of finger pulse oximeters to function well for individuals with dark skin tones.
The FDA has noted that most current scientific evidence shows accuracy differences in pulse oximeters between dark and light skin pigmentation. This is especially concerning as the difference is typically small at saturations above 80% and greater when saturations are less than 80; which is when it is most crucial that patients receive accurate measurements to diagnose life-threatening conditions such as hypoxemia.
The reason for these discrepancies stems from how red and infrared light are absorbed and passed through the body. The graph below is from a study done by The New England Journal of Medicine and shows the extent of this discrepancy when measuring arterial oxygen saturation for White and Black patients. Although the clinical significance of potential racial bias in pulse oximetry measurement is still unknown, the study does conclude that Black patients had nearly three times the frequency of occult hypoxemia that was not detected by pulse oximetry as White patients.
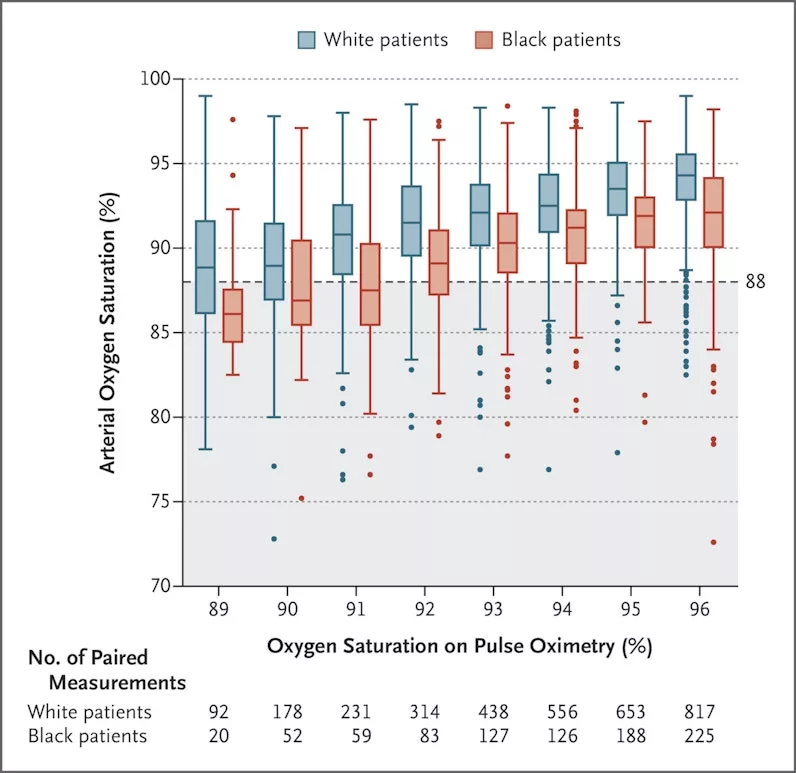
Sourced from, “Racial Bias in Pulse Oximetry Measurement”.
Inaccurate readings can oftentimes be more detrimental than no readings at all. Pulse oximeters tend to overestimate the oxygen saturation of Black patients, which means that low oxygen levels may be missed, causing Black patients to be less likely to receive appropriate oxygen therapy or other medical care when they need it.
An article from the University of Michigan’s Institute for Healthcare Policy and Innovation estimates that these oxygenation miscalculations may result in as many as 1 in 10 inaccurate readings among Black patients. Considering the danger of untreated hypoxia, especially during the COVID-19 pandemic, the extent to which biased pulse oximeters may have delayed appropriate treatment for Black patients is unknown.
So how is it that so many pulse oximeters received FDA validation when they have such serious deficits in capability when monitoring the blood oxygenation of patients with darker skin tones? The answer lies in the studies that evaluated the capabilities of these devices and the subject recruitment bias within these clinical trials.
Case Study: Biases in Scientific Research & Treatment
Bias in clinical studies, particularly regarding race and gender, is a persistent cause of healthcare disparities. The disproportionate representation of minority groups in clinical trials, when compared to their over-represented counterparts, often leads to erroneous study conclusions, poor quality of diagnosis, and potentially dangerous levels of undertreatment.
The 14th American Association for Cancer Research (AACR) Conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved reported the results of a simulated pancreatic cancer clinical trial screening process, in which Black patients were significantly more likely to be excluded from pancreatic clinical trials than their white counterparts. This outcome was not exclusive to oncology studies and extends into many alternative areas of healthcare management, one of which being the field of cardiovascular disease.
Heart conditions, like congestive heart failure, disproportionately affect Black patients due to a higher prevalence of risk factors in that group, such as high blood pressure, obesity, and diabetes. Despite this, the FDA’s Global Participation in Clinical Trials report found that African Americans only accounted for 2.5% of cardiology clinical trial participants.
It’s not only within clinical trials that these biases are seen. A study published by Nature Communications, a peer-reviewed scientific journal, found that when clinicians were presented with standardized videos of either a White male actor or a Black female actor (of similar age, wearing the same attire, and in the same clinical setting) portraying a patient with clinically significant chest pain symptoms, there were significant disparities in the treatment recommendations given to the white male patient-actor and Black female patient-actor. When translated into real clinical scenarios this would then result in the Black female patient being significantly more likely to receive unsafe undertreatment, rather than the guideline-recommended treatment.
Racial and gender biases in clinical treatment recommendations and studies have been a long-standing issue that many researchers and clinicians have tried to address through varied methods. Until a solution is found, however, the death gap will continue to be a challenge unique to the underprivileged and underserved communities in America.
Bringing Clinical Care Home
There are innumerable reasons why patients do not get the healthcare that they need. For many, it is due to factors beyond their control – such as financial strain or an inability to travel long distances. However, the benefits of proactively managing healthcare are considerable. So how can we begin to dismantle these unjust healthcare barriers?
Casana’s new category of effortless, patient-centered technology captures important health parameters like heart rate and blood oxygenation in the comfort of a patient’s home. The Heart Seat™ aims to passively monitor a patient’s health trend without putting additional strain on the user.
Innovative advancements in remote patient care present a unique opportunity to help bridge the ‘death gap’ and associated systemic inequalities in the US healthcare system. Casana is dedicated to improving access to proactive and predictive care to reduce these healthcare disparities and support bridging the ‘death gap’.
To learn more, or for opportunities to get involved, please reach out to info@casanacare.com.
Recommended insights
The man who invented a smart toilet seat
So much of our biological processes are still complete mysteries. It’s so inspiring as someone who loves to solve problems and is not afraid of a challenge. Ninety percent of startups fail, whether that is due...Read More
Why a Smart Toilet Seat is the Unsung Hero of Effortless Technology for Seniors
For seniors who have reached the point of ease over effort, the future of heart health monitoring is sitting right underneath you. Effortless technology is more than just a convenience; it's a catalyst for a paradigm...Read More
Why Agility in Quality Management Systems is Vital
A good quality system is the backbone of any organization.
