Many people have heard the term EKG—but what is it really? An electrocardiogram, abbreviated simply as ECG or EKG, is a non-invasive way to measure and evaluate certain heart health parameters. As the name suggests, an electrocardiogram uses electrodes placed on the skin to measure the electrical activity of your heart – resulting in a graph of voltage versus time. Changes or abnormalities in the EKG pattern are essential to the early detection of heart-related conditions and are one of the most simple and efficient non-invasive tests available to clinicians.
EKG vs ECG
Is an EKG the same as an ECG? Yes, electrocardiogram is commonly abbreviated as both EKG and ECG. The origin of the term “EKG” is simple. In the medical industry, abbreviations are commonplace. Naturally, many abbreviations seem and sound similar to one another. For example, EEG, the abbreviation for electroencephalogram—a test that measures the electrical activity in the brain—resembles ECG. To mitigate the risk of any misunderstandings between EEG and ECG, especially in hectic medical environments, it became common practice to use the German abbreviation of electrocardiogram, EKG, which stands for elektrokardiogramm, to further distinguish between the two tests.
How does an electrocardiogram work?
The heart is a muscle that contracts and relaxes in order to pump blood throughout the body. The movement of the heart is caused by electrical impulses as cells transmit an electrical charge, causing the heart to contract in one coordinated motion, creating what we know as a heartbeat. An electrocardiogram detects this electrical impulse, or “wave”, as it moves through the chambers of the heart with each beat and records it in graphical form.
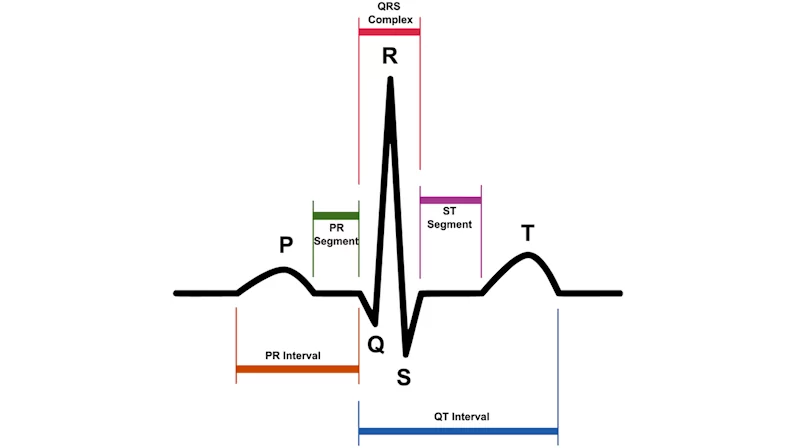
According to the American Heart Association, a normal, healthy heartbeat, as shown on an EKG, will reflect the timing of the upper and lower chambers of the heart’s conduction system. The conduction system in the right and left atria—the upper chambers of the heart—are measured in the P-wave. After the P-wave is a short, flat line that represents the shift of the electrical impulses to the bottom chambers of the heart. The QRS complex is the next portion of an EKG and it gauges how the “wave” travels to the right and left bottom ventricles of the heart. Finally, the T-wave represents the ventricles’ return to a resting state otherwise known as electrical recovery.
“Leads”
A traditional EKG uses sensors that are attached to the skin to detect the electrical signals produced by your heart each time it beats, these sensors are referred to as electrodes. ECG leads are computed by analyzing the electrical currents detected between any two electrodes. The resulting signals are then recorded by a machine and analyzed by health professionals. The most common EKG is a 12-lead EKG.
The 12-lead ECG results in a tracing (a graph of the electrical activity of the heart) from 12 different “electrical positions” of the heart. Each lead is placed in order to detect electrical activity from different positions around the heart. This results in a tracing in which an experienced interpreter would be able to see the heart’s activity from many different angles. Alternative EKGs such as Lead I, Lead II, Lead III, etc., all have their own respective occasions for use, depending on what your doctor or physician may be looking for.
How do cardiologists evaluate an EKG?
Cardiologists and physicians use EKGs to determine two crucial aspects of a patient’s heart health, the time it takes for the electrical wave to pass through various parts of the heart, and the shape of the electrical activity as it passes through the muscle of the heart. Measuring the time intervals between heartbeats on an EKG can help determine if the rhythm of the heart is normal, slow, fast, or irregular. Similarly, the amount of electrical activity passing through the heart can suggest if parts of the heart are too large or potentially overworked. Essentially, an electrocardiogram is a basis for determining if the heart is functioning under normal conditions or if there are any abnormalities.
How do you know if you need an EKG?
Doctors recommend an EKG as a standard diagnostic tool for a variety of issues and concerns. According to Hopkins Medicine, conditions that may warrant an EKG include:
- To determine the cause of chest pain
- To evaluate problems that may be heart-related, such as severe tiredness, shortness of breath, dizziness, or fainting
- To identify irregular heartbeats
- To help ascertain the overall health of the heart before or after procedures/treatments such as surgery
- To see how an implanted pacemaker is working
- To detect how well certain heart medicines are working
- To get a baseline tracing of the heart’s function during a physical exam; this may be used as a comparison with future ECGs, to determine if there have been any changes. (This is also known as trend analysis.)
EKG Limitations
An EKG can be used to diagnose conditions such as abnormal heart rhythms (arrhythmias), blocked or narrowed arteries in your heart (coronary artery disease), heart attack (myocardial infarction), as well as a variety of other heart dysfunctions. Still, an echocardiogram is not the end-all, be-all for cardiovascular testing. With certain conditions, such as heart failure or valvular heart disease (VHD), additional tests, such as an echocardiogram, are required to make a definitive diagnosis. An EKG is oftentimes the first-line test to evaluate the heart health of a patient.
Casana unlocks an effortless medical-grade EKG
EKGs that utilize gel or wet electrodes to measure the electrical activity of the heart has been the traditional standard within medical practices for over one hundred years. They are prioritized as a noninvasive alternative to the implantable loop recorders available, and recent advancements in medical research have made EKGs easier than ever. Today, we find EKGs in wearables and other IoT (Internet of Things) devices that are accessible to people outside of the hospital setting.
Casana is developing a new category in healthcare technologies that enable effortless, integrated, and consistent in-home health monitoring. Casana’s first product, The Heart Seat™ is an IoT health-monitoring toilet seat that measures clinical values through the utilization of the Seat’s sensors. The Heart Seat includes a photoplethysmogram, ballistocardiogram, as well as an echocardiogram. Casana’s mission is to assist medical teams in their care management of patients beyond the four walls of the hospital.
Disclaimer: All of the material provided above is for informational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recommended insights
Boldly Growing: A Start-Up Founder’s Guide to Sustainable Success
Austin led the company through its acquisition by Vista Equity Partners in 2017, and subsequent $4B+ IPO in 2020. Austin is a Forbes 30 Under 30, was named Ernst & Young Technology Entrepreneur of the Year in 2016, and earned recognition as one of the nation's top 50 philanthropists in 2017.
Austin McChord, CEO of Casana, On Stepping Outside Your Comfort Zone
Interview with Austin McChord, CEO of Casana
Casana Appoints New CTO To Accelerate Technological Innovation in Remote Patient Monitoring
Veteran in the medical device space, Samir Zahine, adds significant expertise in product development with FDA compliance