What is SpO2?
The human body is a medical marvel. The brain is capable of regulating the body down to the most minute of details; even the amount of oxygen in our blood—or more specifically, our hemoglobin—requires very precise regulation. Hemoglobin, abbreviated as Hb or Hgb, is a protein in red blood cells capable of carrying oxygen from the respiratory organs to the rest of the body. SpO2, otherwise known as blood oxygenation, is the fraction of oxygen-saturated hemoglobin relative to total hemoglobin in the blood. It is usually denoted as a percent, up to 100% (normal saturation levels in the average adult are 95–100 percent).
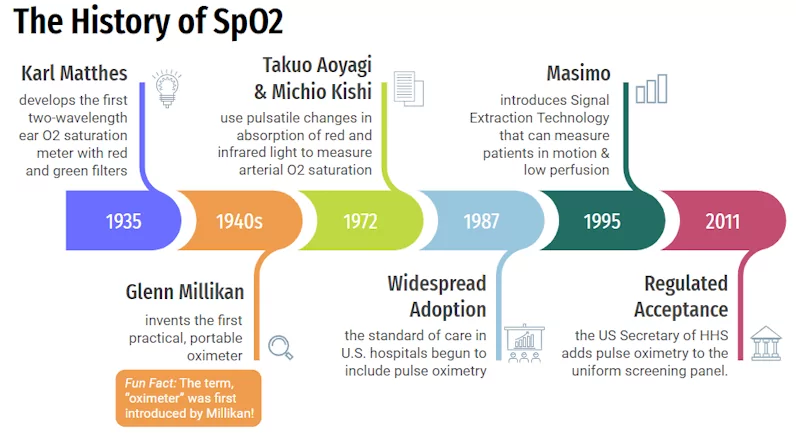
History of Pulse Oximeters
Pulse oximetry, or SpO2, can be said to have originated from the developments that Johann Lambert (1728-1777) and August Beer, Ph.D. (1825-1863) made while advancing and expanding upon the known laws of general oximetry.
- Lambert’s Law: light absorption is proportional to the thickness of a sample
- Beer’s Law: the absorption of light is proportional to the concentration of a sample
By utilizing these laws, the basis for how oximetry—and eventually pulse oximetry—works was established.
It was ultimately discovered that oxygenated hemoglobin (oxyhemoglobin) allows red light to pass through, and absorbs more infrared light, while deoxygenated hemoglobin (deoxyhemoglobin) allows infrared light to pass through, and absorbs more red light. Due to this natural phenomenon, it is possible to send red and infrared light through the body (most commonly through the finger, and less commonly through the thigh) to determine what percentage of the hemoglobin in the blood is oxygenated.
It’s important to note that pulse oximetry is still an imperfect science. Results may not be as accurate for people with darker skin pigmentation due to how red and infrared light are absorbed and passed through the body. The FDA warns that while pulse oximetry is useful for estimating blood oxygen levels, pulse oximeters have limitations and risk of inaccuracy under certain circumstances that should always be considered. Those who check their own oxygen levels, or have others check for them, should bear this in mind when considering results.
A Timeline:
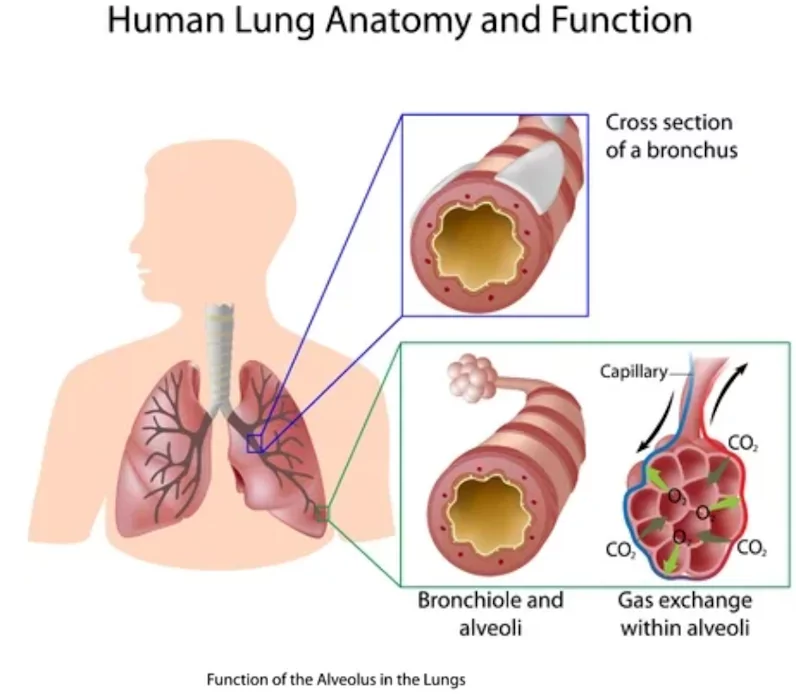
The Lungs and Normal SpO2 levels
So where does the hemoglobin in our blood get this oxygen? Every time you breathe, a complex process takes place as your body inhales air containing oxygen, regulates its temperature and moisture, and then exhales carbon dioxide. This air will move through the windpipe, pass through the bronchi and eventually reach the air sacs. These air sacs, called alveoli, are responsible for gas exchange.
How the Body uses Oxygen
Most people can recall learning about photosynthesis early on in their education; plants receive energy directly from sunlight and convert it into carbohydrates (sugar molecules), which are then used to fuel life-sustaining activities. Oxygen is produced as a waste product of this process, much like how humans produce carbon dioxide. Although humans cannot mimic photosynthesis absolutely, we do similarly use the energy stored in carbohydrates as fuel for our bodies.
In order to acquire energy, we need carbohydrates, which are sourced from green plants, or animals that have eaten green plants. After digestion, sugars are transported to the cells by blood, where the mitochondria (the powerhouse of the cell responsible for energy production) will then break up their chemical bonds to release the energy they contain, using the oxygen provided by the lungs.
What is Normal?
For the average adult, a SpO2 reading between 95 to 100% is within the normal range. Those with breathing-related health conditions such as chronic lung disease or sleep apnea might have normal levels of around 90%. Regularly monitoring your SpO2 levels is the best way to determine what is normal for you. For the average adult, SpO2 readings below 92% are a sign that it is time to speak with your healthcare provider.
Why Measure SpO2
A SpO2 level of 92% or lower can indicate potential hypoxemia, a seriously low level of oxygen in the blood which requires medical treatments such as external oxygen supplementation. If oxygen levels remain low or continue to worsen, the condition may evolve into a more serious condition called hypoxia. The most proactive way to know if you are at risk of hypoxemia or hypoxia is by checking your oxygen saturation levels regularly. If you are concerned about your oxygen saturation levels, regularly monitoring and sharing the readings that you receive (as well as the date and time of those readings) can help doctors evaluate your condition.
Symptoms of Hypoxemia
Hypoxemia can occur when oxygen levels in the blood are lower than normal, which may inhibit necessary bodily functions. Mild symptoms of hypoxemia include headaches and shortness of breath. However, it can interfere with heart and brain function in more severe cases.
Additional symptoms such as fast heartbeat, coughing, wheezing, confusion, & bluish color in skin, fingernails, and lips are also signs of hypoxemia.
Symptoms of Hypoxia
When prolonged hypoxemia causes low oxygen levels in your body’s tissues we refer to that as hypoxia. Occasionally, these two terms are used interchangeably, but they are not the same thing. The symptoms of hypoxia will often mirror those seen in hypoxemia; contact your doctor if you experience the symptoms listed above. Early diagnosis and treatment can help ensure the condition does not get worse and cause dangerous complications.
Diseases that affect SpO2
It is particularly important to measure oxygen saturation in patients with health conditions that reduce the level of oxygen in the blood. Some examples of these conditions include chronic obstructive pulmonary disease (COPD), asthma, pneumonia, lung cancer, anemia, heart failure, heart attack, and other cardiopulmonary disorders.
COVID and Oxygen Saturation
COVID-19 can negatively impact an individual’s ability to breathe and absorb the necessary oxygen to support life-sustaining functions. Those who test positive for COVID-19 often have lower levels of oxygen saturation, and although some may not be able to feel this difference, those with preexisting conditions often struggle due to the diminished lung capacity.
While a pulse oximeter can measure a patient’s oxygen saturation, it is not recommended as a method to diagnose COVID-19. Monitoring your SpO2, however, is a great way to track any health trends that may be indicative of a greater medical need. COVID-19 has also been cited as causing a phenomenon called “silent hypoxemia” or “happy hypoxia,” where a patient shows little to no symptoms but still has low blood oxygen levels.
Those with COVID-19—whose symptoms are mild and do not require medical intervention—are advised to track their blood oxygen saturation over time as it may help medical professionals measure the progression of the disease.
Finger Pulse Oximeters
Although there are many devices on the market that allow consumers to measure their pulse oxygenation (fitness trackers, smart watches, and wrist cuffs to name a few) the most well-known form of pulse oximetry is the finger pulse oximeter. Finger pulse oximeters measure how much red and infrared light passes through your fingertip in order to estimate what proportion of your red blood cells are carrying oxygen. The popularity of these devices is mainly derived from their ease of use, relatively low price point, and general accuracy (which may differ from one device to another). Due to these factors, as well as the usefulness of the data these devices provide to clinicians, finger pulse oximeters have become a common option for at-home SpO2 monitoring.
Of course, finger pulse oximeters face challenges of their own. Some common factors that can reduce the accuracy of pulse oximeter readings include poor circulation, skin temperature, skin thickness, current tobacco use, use of fingernail polish, and dark skin pigmentation, according to the FDA. Beyond accuracy, the real value of health monitoring lies in the ability to share this data with physicians and care team members to facilitate the development of actionable insights.
The Future of SpO2 Monitoring
Effortless in-home monitoring that overcomes adherence issues – by requiring no behavior change from a user – is the next step toward the advancement of healthcare. Casana believes that The Heart Seat™ can positively impact blood oxygenation management, as well as a myriad of other conditions. Empowering patients to participate in, and better manage their health care starts with enabling them to overcome the adherence barriers that plague traditional devices. When used by clinicians, remote patient monitoring solutions, such as The Heart Seat, can provide a more holistic view of a patient’s health over time, support medication management, and enable timely intervention before a costly care episode.

Casana’s new category of effortless, patient-centered technology captures important health parameters like blood oxygenation without requiring any change in behavior. Instead of often expensive wearable gadgets, which many people abandon shortly after purchase, The Heart Seat aims to passively monitor a patient’s health and seeks to reliably track trends and insights unobtrusively. Consistently monitoring vital signs can be an integral piece of management for those at risk or who show early signs of relevant health conditions. We believe our technology represents a cost-effective medical technology that will help enable doctors to determine the best course of action to improve patient outcomes and experiences.
Recommended insights
How A Smart Toilet Seat Can Empower Older Adults to Age in Place with Confidence
Imagine a toilet seat that monitors your health behind the scenes. That's the power of a smart toilet seat, especially for older adults looking to age in place with integrity. Don’t believe us? In a recent...Read More
Predicting the Unpredictable | How Managing the Supply Chain at a Startup is Full of Exciting Challenges
Interview with Shannon Clements, Supply Chain Manager at Casana
Managing Heart Failure Symptoms During the COVID-19 Pandemic
Without question, the Pandemic has created great upheaval in almost every aspect of our lives. One of the most concerning consequences is that many patients are too afraid to go to the hospital for life saving...Read More
