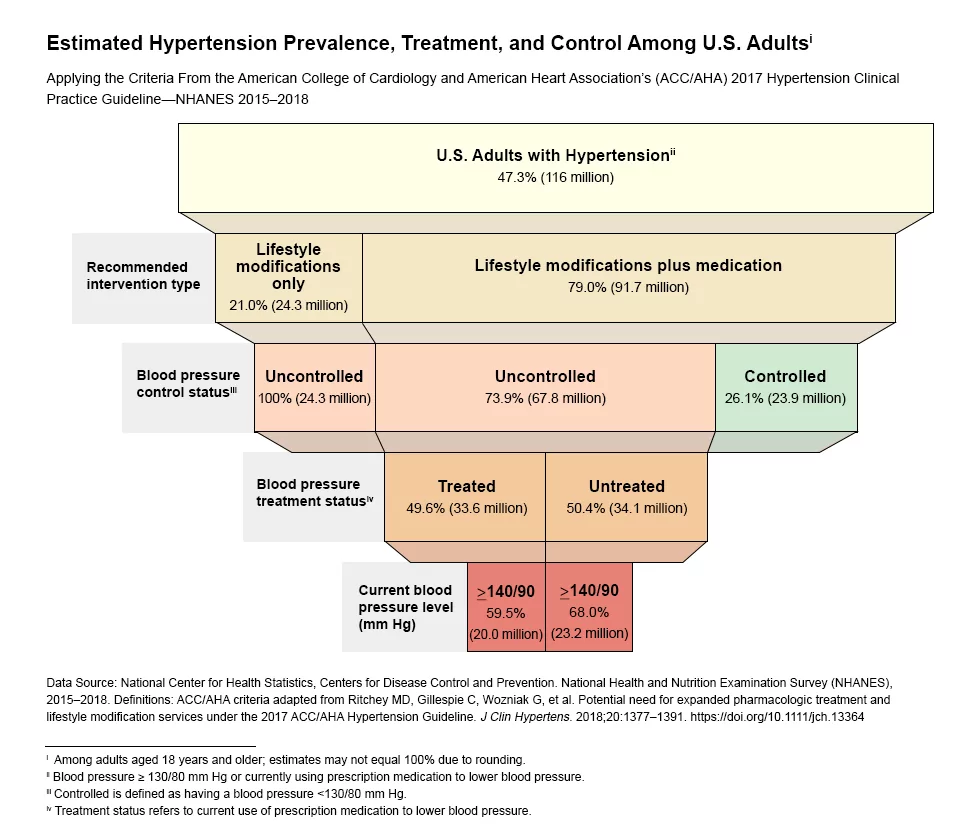
Hypertension, more commonly known as high blood pressure (BP), in adults, is usually defined as “systolic blood pressure (SBP) of 140 Hg or higher, or diastolic blood pressure (DBP) of 90 mm Hg or higher” by the United States Preventive Services Task Force (USPSTF). Nearly half of the adults in the United States (108 million, or 45%) have hypertension, while one-third of Americans with high blood pressure don’t even know it, and over half of US adults with hypertension do not have it under control, neglecting to take medication regularly. According to the CDC, in 2018 nearly 500,000 deaths in the United States included high blood pressure as a primary or contributing cause. This is why the early detection of high blood pressure is a crucial aspect of health management.
Although less prevalent than hypertension, it is also important to note that low blood pressure, also known as hypotension, is another significant driver for monitoring blood pressure in the home. Understanding hypertension and its associated health risks can help make the stress and uncertainty of a hypertension diagnosis feel more manageable. There are many excellent hypertension resources available online. In this post, we’ll explain the basics.
What is Hypertension
While traveling through the circulatory system, blood pushes against the sides of the arteries and vessels with varying degrees of strength. This pressure is called blood pressure and when blood pressure is consistently too high, it is referred to as hypertension, or primary (essential) hypertension. Blood pressure is most often indicated by two numbers.
The first is systole, when the heart contracts and ejects blood into the arteries. The second is diastole, when the heart relaxes. The reading is a unit expressed in millimeters of mercury (mmHg). The measurement is most generally written as systolic/diastolic, or “120 / 80 (mmHg)”. As mentioned previously, the United States Preventive Services Task Force generally describes the threshold used to define hypertension as a range from 130/80 mmHg or greater, to 140/90 mm Hg or greater. Secondary hypertension refers to high blood pressure caused by another underlying condition. This type of blood pressure tends to appear suddenly and causes higher blood pressure than primary hypertension.
Some examples of conditions that can lead to secondary hypertension include: obstructive sleep apnea, kidney disease, thyroid problems, and certain medications such as birth control pills or cold remedies.
A systolic pressure of less than 120 and a diastolic pressure of less than 80 is considered normal and healthy, but blood pressure that’s too low (hypotension), in which readings are below 90 mmHg systolic or 60 mmHg diastolic, can also be a cause for concern. Blood pressure must be carefully managed in order to stay within a healthy range.
Early Symptoms of Hypertension
There are very few early symptoms of hypertension and most people with hypertension are often asymptomatic, contributing to why so many cases of hypertension go undiagnosed.
Some possible hypertension symptoms include chest pain, shortness of breath, irregular heartbeat, peripheral edema or swelling, headaches, blurred vision, sweating, nosebleeds, nausea, and dizziness.
Identifying Hypertension
When a person suffers from hypertension, the walls of their circulatory system are constantly under too much strain.
Whenever possible, the accepted guidance is that a diagnosis should not be based on a single office visit. Typically 2–3 office visits at 1–4-week intervals (depending on the blood pressure levels) are recommended to confirm the diagnosis of hypertension. Diagnosis might be made on a single visit in extreme cases (if BP is ≥ 180 / 110 mmHg) and there is evidence of cardiovascular disease (CVD). According to the AHA “Out-of-office BP measurement is often necessary for the accurate diagnosis of hypertension and for treatment decisions”.
The use of home BP measurements helps to identify individuals with white coat hypertension (elevated BP in the office often due to stress), and those with masked hypertension (non-elevated BP in the office, but elevated BP at home).
Diagnosing hypertension often includes a medical history exam as well as a physical exam. Components of the medical history exam include: historic blood pressure levels, personal risk factors including lifestyle habits such as diet or smoking, as well as family history. The physical exam includes examining: pulse rate, basal crackles, peripheral edema, enlarged kidneys, neck circumference, enlarged thyroid, and increased BMI. Lab tests may also be performed including blood tests to evaluate sodium, potassium, serum creatinine, urine test, and 12-lead ECG to evaluate atrial fibrillation, left ventricular hypertrophy, and ischemic heart disease.
Cost of Hypertension
High blood pressure costs over $50 billion every year just in the United States. Some experts estimate that the number could be over $1 trillion globally. This total includes the cost of healthcare services, medications to treat high blood pressure, and loss of productivity from premature death. A proactive and preventative approach that supports compliance with daily care plans could not only save the healthcare system billions, but it could also save lives. Solutions with a lower financial burden on payers, such as the Heart Seat, hope to help promote affordable and effortless home monitoring which improves the quality of life of those managing hypertension.
Treatment & Managing Hypertension
Individuals identified with confirmed hypertension should receive appropriate pharmacological treatment. Individuals with elevated blood pressure or who are at risk of hypertension should engage in proactive lifestyle changes to proactively manage their blood pressure and prevent or delay the onset of high BP and reduce cardiovascular risk.
The goal of managing hypertension is to bring blood pressure levels back to the “green zone.” Controlling hypertension can take on many forms; there are both proactive lifestyle and reactive pharmacological approaches to managing high blood pressure, but it’s important to remember that for the most part high blood pressure usually has no symptoms. It is for this reason that hypertension is referred to as the silent killer; having high blood pressure puts you at an increased risk for heart disease, heart failure, and stroke, among many other chronic conditions.
Pharmacological Approach
The pharmacological approach to managing high blood pressure is to regularly take the medication prescribed by your doctor. While modern medicine is remarkably effective and capable of controlling hypertension in patients who take their medications as prescribed, on average across the world, less than 50% of adults with hypertension receive BP-lowering medication. This is despite the fact that a difference in BP of 20/10 mmHg is associated with a 50% difference in cardiovascular risk, according to the AHA.
It is also a widely acknowledged fact that “doctors are often slow to make changes to a patient’s drug regimen even when they see blood pressure readings that are clearly outside of the desired range”. In this case, treatment is targeted at regulating high blood pressure and avoiding further health deterioration.
Lifestyle Approach
Proactive lifestyle care takes on the form of managing blood pressure before it becomes a serious threat to your health. Practicing healthy living habits by maintaining a healthy diet and weight, being physically active, sleeping well, and refraining from smoking or drinking in excess can help keep your blood pressure in a healthy range. Even when incorporating all of these lifestyle changes into your daily routine it is also important to monitor your blood pressure. An average of blood pressure readings taken over time is more accurate than one that is taken only once, due to the various external factors that might affect any single measurement, which is why most doctors recommend that patients at risk or currently suffering due to hypertension measure their blood pressure twice a day and keep track of trends over time. Despite these recommendations, it can be an arduous task for patients and doctors to manage.
Patient Adherence
It’s when attempting to introduce daily monitoring into treatment and management plans that patient adherence becomes the largest hurdle from both a doctor’s perspective as well as a patient’s perspective. Taking medication regularly as prescribed and monitoring blood pressure twice a day can become quite time-consuming and for most people can be seen as burdensome, or nearly impossible.
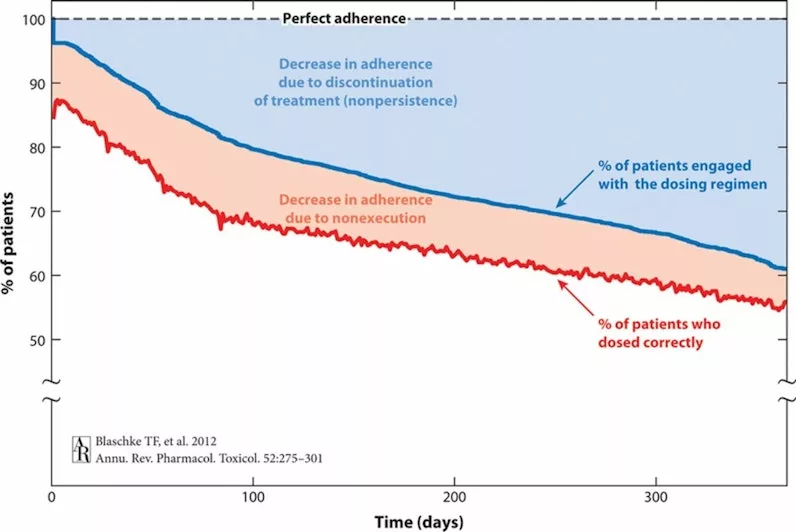
Adherence statistics are shocking. One example of this can be observed throughout ninety-five studies whose data was electronically compiled to monitor the time course of adherence parameters for 36,907 patients prescribed oral medications over the course of a year. They found that “the percentage of patients still engaged with their dosing regimen as time passed after the start of treatment… [declined due to] patients’ permanent discontinuation of their dosing, as they ended their persistence with the prescribed once-daily dosing regimen”. Essentially, it has been shown that few patients perfectly adhere to treatment plans, whether that be medication or monitoring. This is why solutions that circumvent the need for lifestyle changes within the patient population are highly anticipated as the future of healthcare.
Innovation in In-Home Health Monitoring
As technological advancements spur innovation within the healthcare industry, a new form of medical monitoring has emerged, namely telemonitoring. Telemonitoring, otherwise known as remote physiological monitoring (RPM), is technically defined as the use of information technology to monitor patients at a distance. Another way to think about telemonitoring is to reorient the focus of health monitoring to where the person spends the most time, at home. This home health monitoring is highly useful for chronic and long-standing illnesses such as heart disease or hypertension.
Casana’s new category of effortless, patient-centered technology captures important health parameters. Instead of expensive wearable gadgets, which many people abandon shortly after purchase, The Heart Seat™ aims to passively monitor a patient’s health and seeks to reliably track trends and insights unobtrusively. Consistently monitoring vital signs can be an integral piece of management for those at risk or with early signs of hypertension. Having reliable trend data can be invaluable to doctors and care teams when determining the best course of action to take in order to improve patient outcomes and experiences. Few new medical technologies have the potential to do so while also reducing costs. We believe this is one.
DISCLAIMER: The Heart Seat is currently under development for blood pressure measurement. The Heart Seat is NOT FDA cleared for blood pressure at this time.
Recommended insights
Protecting Grandma’s Privacy and Security with Health Tech
In today's digital age, our elders are increasingly turning to health technology solutions to manage their well-being. But with great convenience comes great responsibility—especially when it comes to safeguarding their data. Let's dive into why data...Read More
Boldly Growing: A Start-Up Founder’s Guide to Sustainable Success
Austin led the company through its acquisition by Vista Equity Partners in 2017, and subsequent $4B+ IPO in 2020. Austin is a Forbes 30 Under 30, was named Ernst & Young Technology Entrepreneur of the Year in 2016, and earned recognition as one of the nation's top 50 philanthropists in 2017.
Why Ballistocardiography is the Leader of Next Generation Cardiac Sensors
A century-old sensor carries the potential to revolutionize today's in-home care. The BCG's potential has been rediscovered.
