Most adults with hypertension in the United States are recommended prescription medication with lifestyle modifications (91.7 million). Many who are already treated with hypertension medication may need to have their current medication dosage increased or to be prescribed additional medications to achieve blood pressure control (33.6 million). Controlling hypertension, or high blood pressure, is difficult due to the various health conditions that could be causing it. Doctors trying to prescribe medication to assist with hypertension management often have to go through a trial and error period, prescribing multiple types of medication in order to determine which works best for a particular patient.
Hypertension medication can be a confusing topic even for physicians. With there being over ten classes of blood pressure medication, many of which are taken in conjunction with one another, understanding the basics of hypertension medication can seem like a daunting task. Over the course of the post, we will go over the classes of medication, their use, and other relevant information as provided by the American College of Cardiology (ACC) and American Heart Association (AHA) Task Force within the 2017 Hypertension Guidelines.
When to Medicate:
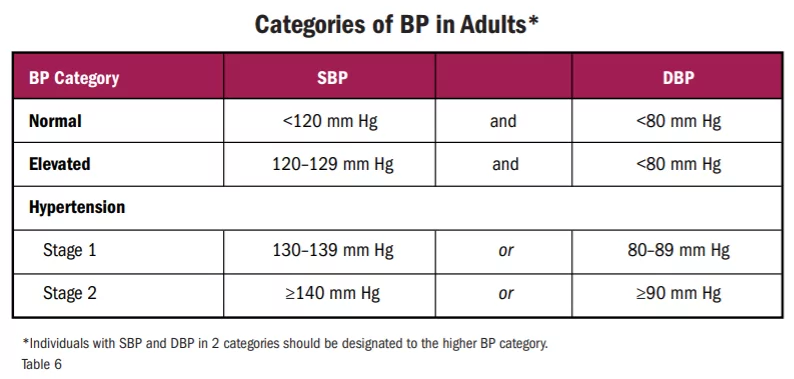
There are four distinct categories of blood pressure in adults as defined by the ACC & AHA, Normal, Elevated, Stage One Hypertension, and Stage 2 Hypertension. We will briefly go over the blood pressure thresholds and recommendations for treatment and follow-up.
Normal Blood Pressure
Patients with systolic blood pressure (SBP) under 120 mm Hg and less than 80 mm Hg diastolic blood pressure (DBP) can be classified as those with normal BP. At this point, a physician only needs to continue to promote optimal lifestyle habits and reassess the patient’s condition in a year.
Elevated Blood Pressure
Once systolic blood pressure increases above 120 mm Hg (but remains under 130 mm Hg) while maintaining a diastolic BP under 80 mm Hg, a patient can be classified to have Elevated BP. Once it has been determined that these readings are not Secondary Hypertension or White Coat Syndrome, the first course of action is to recommend nonpharmacologic therapy such as diet, exercise, lower sodium intake, etc. The patient’s health should be reassessed in three to six months.
Secondary Hypertension: high blood pressure that’s caused by another medical condition.
White Coat Syndrome: a disorder in which a person develops high blood pressure when they are around doctors, who often wear white coats.
Stage One Hypertension
A systolic blood pressure of 130 mm Hg and above (up to 139 mm Hg) in concurrence with a diastolic blood pressure of 80 mm Hg to 89 mm Hg indicates Stage One Hypertension. Once a patient is diagnosed with Stage One Hypertension it is crucial that their doctor perform an ASCVD (atherosclerotic cardiovascular disease) risk assessment. If the patient scores 10% or less it is safe* to attempt nonpharmacologic therapy and reassess in three to six months. If their score is greater than 10% a doctor should continue to recommend nonpharmacologic therapy in addition to BP-lowering medication.
Once BP-lowering medication has been prescribed, a reassessment should happen in one month’s time. If the BP goal set by the doctor is met, the patient should continue using their prescribed medication while following their nonpharmacologic therapy routine and make sure to check in with their doctor for reassessment every three to six months. If the BP goal is not met, doctors should assess and optimize adherence to therapy, consider intensification of the therapy, and then reassess in one month.
ASCVD Risk Score: a national guideline developed by the American College of Cardiology. It is a calculation of your 10-year risk of having a cardiovascular problem, such as a heart attack or stroke.
*Note that patients with DM or CKD are automatically placed in the high-risk category.
Stage Two Hypertension
Once systolic blood pressure is higher than 140 mm Hg and diastolic BP has reached 90 mm Hg, the patient can be classified to have Stage Two Hypertension. There is no need to conduct the ASCVD risk assessment, doctors should institute nonpharmacologic therapy and BP-lowering medication immediately and reassess in one month. Assessment of the success of BP-lowering medication is the same as outlined in the Stage One Hypertension section above.
Classes of Medication
Hypertension medications, also known as antihypertensives, are capable of lowering high blood pressure once prescribed. There are eleven classes of blood pressure medication and within these classes there are subclasses. Talk to your doctor before making any medical decisions, and never stop taking a prescribed medication or change your dose or frequency without first consulting your doctor.
For in-depth information on generic and brand-name antihypertensives, visit the American Heart Association website.
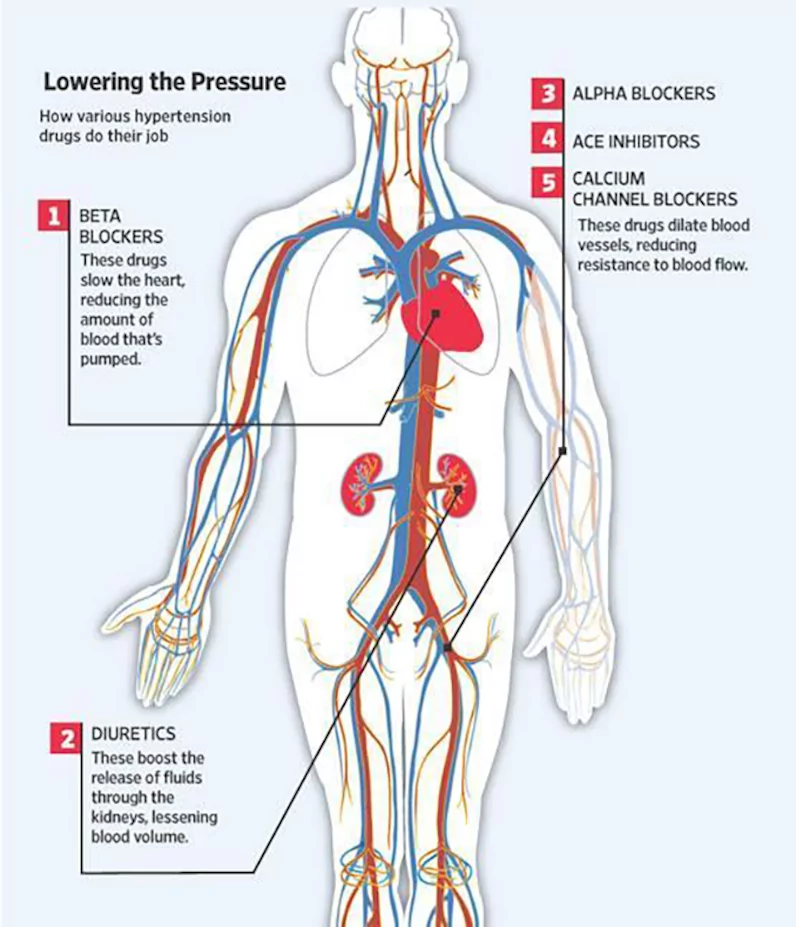
1. Diuretics
Diuretics help the body get rid of excess sodium (salt) and water and help control blood pressure. They are often used in combination with additional prescription therapies.
Diuretics can be further divided into:
- Thiazide diuretics
- act directly on the kidneys and promote diuresis (urine flow) by inhibiting the sodium/chloride cotransporter located in the distal convoluted tubule of a nephron (the functional unit of a kidney).
- Potassium-sparing diuretics
- are medications that increase diuresis (urination) without the loss of potassium. They are generally weak diuretics and work by interfering with the sodium-potassium exchange in the distal convoluted tubule of the kidneys or as an antagonist at the aldosterone receptor.
- Loop diuretics
- are a powerful type of diuretic that work by inhibiting the sodium-potassium-chloride (Na+/K+/2Cl) co-transporter in the thick ascending loop of Henle, which is located in the kidneys.
- Combination diuretics
- are the utilization of more than one subclass of diuretics. Several combinations have been used; however, the combination of a loop diuretic and a thiazide drug acting on the distal tubule appears to be the most effective.
Potential Side Effects Include:
- Some of these drugs may decrease your body’s supply of the mineral potassium. Symptoms such as weakness, leg cramps, or tiredness may result.
- Some people suffer from attacks of gout after prolonged treatment with diuretics. This side effect isn’t common and can be managed by other treatments.
- People with diabetes may find that diuretic drugs increase their blood sugar levels.
- Impotence may occur.
Some common brand-name diuretics include: Hygroton, Diuril, Esidrix, Hydrodiuril, Microzide, Midamar, Aldactone, Dyrenium, Lasix, Bumex, Moduretic, Aldactazide, Dyazide, Maxzide, etc.
The generic names of commonly used diuretics include: chlorthalidone, chlorothiazide, hydrochlorothiazide, amiloride hydrochloride, spironolactone, triamterene, furosemide, bumetanide, etc.
2. Beta-Blockers
Beta-blockers reduce the heart rate, the heart’s workload, and the heart’s output of blood, which lowers blood pressure.
Beta-Blockers can be further divided into:
- Cardioselective
- Beta-adrenergic blocking agents prevent stimulation of the beta-1 adrenergic receptors at the nerve endings of the sympathetic nervous system and therefore decrease the activity of the heart.
- Cardioselective and Vasodilatory
- Induces nitric oxide-induced vasodilation, which dilates blood vessels and therefore decreases blood pressure.
- Noncardioselective
- Beta-adrenergic blocking agents prevent stimulation of the beta adrenergic receptors at the nerve endings of the sympathetic nervous system and therefore decrease the activity of the heart.
- Intrinsic Sympathomimetic Activity
- Stimulate beta-adrenergic receptors (agonist effect) and oppose the stimulating effects of catecholamines (antagonist effect) in a competitive way.
Potential Side Effects Include:
- Insomnia
- Cold hands and feet
- Tiredness or depression
- Slow heartbeat
- Symptoms of asthma
- Impotence may also occur
Some common brand-name beta-blockers include: Sectral, Tenormin, Kerlone, Zebeta, Cartrol, Lopressor, Toprol-XL, Corgard, Levatol, Visken, Inderal, Betapace, Blocadren, etc.
The generic names of commonly used beta-blockers include: acebutolol, atenolol, betaxolol, bisoprolol fumarate, carteolol hydrochloride, metoprolol tartrate, metoprolol succinate, nadolol, etc.
3. ACE Inhibitors
Angiotensin is a chemical that causes the arteries to become narrow throughout the body, but especially in the kidneys. ACE stands for Angiotensin-converting enzyme. ACE inhibitors help the body produce less angiotensin, which helps the blood vessels relax and open up, which, in turn, lowers blood pressure.
Potential Side Effects Include:
- Skin rash
- Loss of taste
- Chronic dry, hacking cough
- In rare instances, kidney damage
Some common brand-name ACE Inhibitors include: Lotensin, Capoten, Vasotec, Monopril, Prinivil, Zestril, Univasc, Aceon, Accupril, Altace, Mavik, etc.
The generic names of commonly used ACE Inhibitors include: benazepril hydrochloride, captopril, enalapril maleate, fosinopril sodium, lisinopril, moexipril, perindopril, quinapril hydrochloride, ramipril, etc.
4. Angiotensin II Receptor Blockers
These drugs block the effects of angiotensin, a chemical that causes the arteries to become narrow. Angiotensin needs a receptor- like a chemical “slot” to fit into or bind with- in order to constrict the blood vessel. ARBs block the receptors so the angiotensin fails to constrict the blood vessel. This means blood vessels stay open and blood pressure is reduced.
Potential Side Effects Include:
- May cause occasional dizziness.
- ARBs should not be used during pregnancy.
Some common brand-name ARBs include: Atacand, Teveten, Avapro, Cozaar, Micardis, Diovan, etc.
The generic names of commonly used ARBs include: candesartan, eprosartan mesylate, irbesartan, losartan potassium, telmisartan, valsartan, etc.
5. Calcium Channel Blockers
This drug prevents calcium from entering the smooth muscle cells of the heart and arteries. When calcium enters these cells, it causes a stronger and harder contraction, so by decreasing the calcium, the hearts’ contraction is not as forceful. Calcium channel blockers relax and open up narrowed blood vessels, reduce heart rate, and lower blood pressure.
Calcium Channel Blockers (CCB) can be further divided into:
- Dihydropyridines
- are arterial-specific vasodilators of peripheral resistance arteries that cause generalized vasodilation, including the renal, cerebral, intestinal, and coronary vascular beds.
- Nondihydropyridines
- Nonselective inhibitors of L-type calcium channels can reduce myocardial contractility, slow heart rate, and slow conduction, therefore decreasing blood pressure.
Potential Side Effects Include:
- Palpitations
- Swollen ankles
- Constipation
- Headache
- Dizziness
Some common brand-name CCBs include: Norvasc, Lotrel, Vasocor, Cardizem CD, Cardizem SR, Dilacor XR, Tiazac, Plendil, DynaCirc, DynaCirc CR, Cardene SR, Adalat CC, Procardia XL, etc.
The generic names of commonly used CCBs include: amlodipine besylate, bepridil, diltiazem hydrochloride, felodipine, isradipine, nicardipine, nifedipine, nisoldipine, etc.
6. Alpha-1 Blockers
Alpha-1 Blockers reduce the arteries’ resistance, relaxing the muscle tone of the vascular walls.
Potential Side Effects Include:
- Fast heart rate
- Dizziness
- A drop in blood pressure when you stand up
Some common brand-name alpha-1 blockers include: Cardura, Minipress, Hytrin, etc.
The generic names of commonly used alpha-1 blockers include: doxazosin mesylate, prazosin hydrochloride, terazosin hydrochloride, etc.
7. Alpha-2 Receptor Agonists
Alpha-2 Receptor Agonists reduce blood pressure by decreasing the activity of the sympathetic (adrenaline-producing) portion of the involuntary nervous system. Methyldopa is considered a first-line antihypertensive during pregnancy because adverse effects are infrequent for the pregnant woman or the developing fetus.
Potential Side Effects Include:
- Methyldopa (a generic drug type) can cause drowsiness or dizziness
Some common brand-name alpha-2 receptor agonists include: Aldomet, Catapres, Catapres-TTS, etc.
The generic name(s) of commonly used alpha-2 receptor agonists include: methyldopa, Clonidine, Clonidine patch, etc.
Combined Alpha and Beta-Blockers
Combined alpha and beta-blockers are used as an IV drip for those patients experiencing a hypertensive crisis. They may be prescribed for outpatient high blood pressure use if the patient is at risk for heart failure.
Potential Side Effects Include:
- May cause a drop in blood pressure when you stand up
Some common brand-name combined alpha and beta-blockers include: Coreg, Normodyne, Trandate, etc.
The generic names of commonly used combined alpha and beta-blockers include: carvedilol, labetalol hydrochloride, etc.
8. Central Agonists
Central agonists also help decrease the blood vessels’ ability to tense up or contract. The central agonists follow a different nerve pathway than the alpha and beta-blockers but accomplish the same goal of blood pressure reduction.
Potential Side Effects Include:
- Alpha methyldopa may produce a greater drop in blood pressure when you’re in an upright position. This drug may also cause drowsiness or sluggishness, dryness of the mouth, fever or anemia. Male patients may experience impotence.
- Clonidine, guanabenz or guanfacine may produce severe dryness of the mouth, constipation or drowsiness.
Some common brand-name central agonists include: Aldomet, Catapres, Wytensin, Tenex, etc.
The generic names of commonly used central agonists include: alpha methyldopa, clonidine hydrochloride, guanabenz acetate, guanfacine hydrochloride, etc.
9. Peripheral Adrenergic Inhibitors
These medications reduce blood pressure by blocking neurotransmitters in the brain. This blocks the smooth muscles from getting the “message” to constrict. Peripheral adrenergic inhibitors are rarely used unless other medications don’t help.
Potential Side Effects Include:
- Reserpine may cause a stuffy nose, diarrhea or heartburn.
- Guanadrel or guanethidine may cause some diarrhea.
Some common brand-name peripheral adrenergic inhibitors include: Hylorel, Ismelin, Serpasil etc.
The generic names of commonly used peripheral adrenergic inhibitors include: guanadrel, guanethidine monosulfate, reserpine, etc.
10. Vasodilators
Blood vessel dilators, or vasodilators, can cause the muscle in the walls of the blood vessels (especially the arterioles) to relax, allowing the vessel to dilate (widen). This allows blood to flow through better.
Potential Side Effects Include:
- Hydralazine may cause headaches, swelling around the eyes, heart palpitations or aches and pains in the joints.
- Minoxidil may cause fluid retention (marked weight gain) or excessive hair growth.
Some common brand-name vasodilators include: Apresoline, Loniten, etc.
The generic names of commonly used vasodilators include: hydralazine hydrochloride, minoxidil, etc.
Prescribing Medication
There are many antihypertensive medications that can be used to control high blood pressure, as shown above, and in most cases, hypertension is accompanied by a comorbidity of some kind which would affect each individual’s prescription needs uniquely. This section will go over the basic decision-making process for determining which hypertension medication is right for a patient according to the 2017 Hypertension Guidelines. We will not be accounting for situations in which additional medications, for treatments other than hypertension, are included in a care plan.
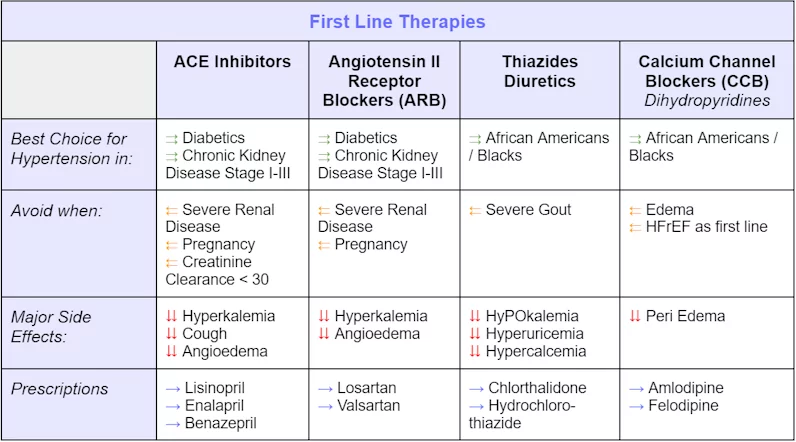
First-Line Therapies
First-line therapies are the initial treatments given to treat a disease. Especially when used individually, first-line therapies are accepted as the best treatment.
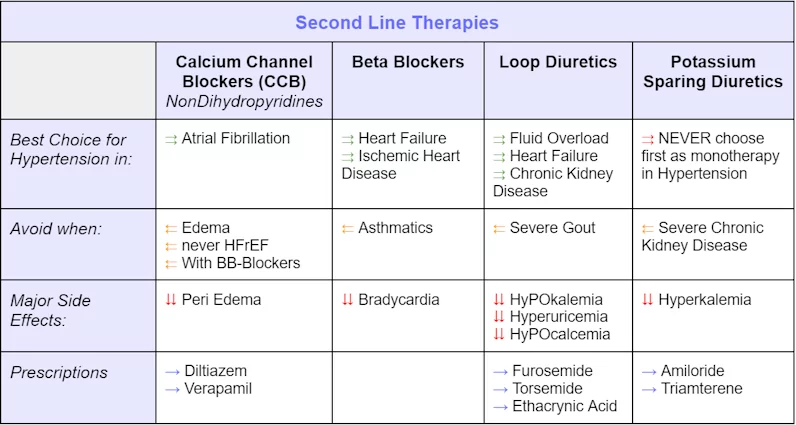
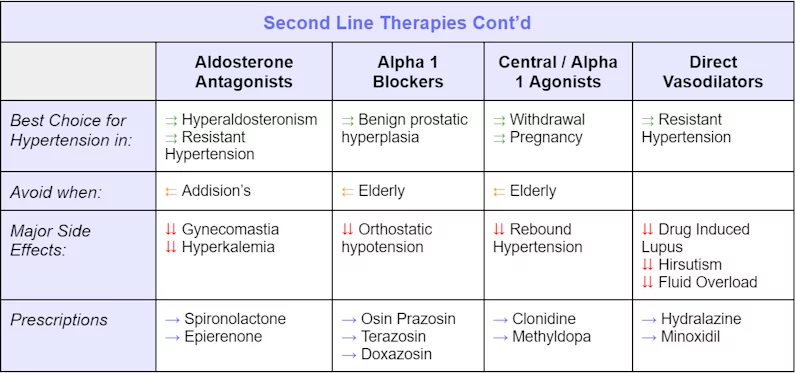
Second-Line Therapies
Second-line and further-line (third, fourth, etc.), therapies are treatment plans for a disease or condition after the initial treatment (first-line treatment) has failed, stopped working, or has side effects that cannot be tolerated.
Disclaimer: All of the material provided above is for informational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. Casana does not endorse any of the products or services mentioned in this post.
Remote Patient Monitoring & Cardiovascular Outcomes
Remote Patient Monitoring, otherwise known as RPM, is the utilization of technology to enable the monitoring of patients outside of conventional clinical settings. The goal of RPM can range from increasing access to care, decreasing healthcare delivery costs, improving outcomes, and more. There is particular interest in the potential of RPM within the cardiovascular field.
The American Heart Association’s position on the utilization of RPM technologies for better cardiovascular disease outcomes is as follows:
Remote patient monitoring (RPM) can empower patients to better manage their health and participate in their health care. When used by clinicians, RPM can provide a more holistic view of a patient’s health over time, increase visibility into a patient’s adherence to treatment, and enable timely intervention before a costly care episode. Clinicians can strengthen their relationships with, and improve the experience of, their patients by using the data sent to them via RPM to develop a personalized care plan and to engage in joint decision-making to foster better outcomes. The American Heart Association supports initiatives that increase access to and incentivize the appropriate design and use of evidence-based remote patient monitoring technologies.
The AHA supports the claim that RPM can reduce systolic and diastolic blood pressure significantly when compared to the usual care and self-monitoring encouraged in conventional clinical settings. Though the results of the research have been largely heterogeneous, and thus inconclusive, The American Heart Association paper which outlines guidance for the utilization of RPM for better cardiovascular outcomes states,
In three-way comparisons, though self-monitoring alone may have a positive impact on blood pressure control compared to usual care, the inclusion of RPM can have a more substantive impact on SBP and DBP than self-monitoring. Additional studies have shown that RPM’s positive impact on SBP can increase if the intervention is long-term.
Casana believes that effortless in-home monitoring can be a solution that results in a positive impact on blood pressure control – particularly supporting the period of titrating medications for patients managing hypertension – as well as a myriad of other conditions, as it overcomes the adherence issues which plague the traditional healthcare system.
For more information on hypertension, antihypertensive medications, and RPM please visit credible websites such as cdc.gov, acc.org, or heart.org or reach out to your primary care provider. If you’d like to connect with Casana sign up for updates or send us a message at info@casanacare.com.
Recommended insights
Toilet Talk: The Supply Chain Significance
Supply chain fluctuations continue to affect the availablity of goods, smart toilet seats included.
In-Home Cardiovascular Monitoring System for Heart Failure: Comparative Study
The study, In-Home Cardiovascular Monitoring System for Heart Failure: Comparative Study, authored by Nicholas J Conn PhD., Karl Q Schwarz MD., and David A Borkholder PhD., was inspired by the demand for solutions that can monitor...Read More
Why a Smart Toilet Seat is the Unsung Hero of Effortless Technology for Seniors
For seniors who have reached the point of ease over effort, the future of heart health monitoring is sitting right underneath you. Effortless technology is more than just a convenience; it's a catalyst for a paradigm...Read More
