Pulse Oximetry: Lighting the Way to Improved Health Monitoring
Published: February 16, 2023
Oxygen, a naturally occurring molecule invisible to the eye, holds incredible value for sustaining life. Tough to see both in the air and in our bodies, oxygen is an important aspect of heart and lung health. In addition to being a natural component for survival, doctors often need to monitor blood oxygen levels in order to better treat patients.
A traditional method of recording blood oxygenation typically involves drawing arterial blood samples; a process similar to how individuals donate blood. This method can be both painful and time consuming, requiring at least 15 minutes to analyze. Pulse oximetry, on the other hand, utilizes the power of light to obtain results instantaneously and without discomfort.
Pulse Oximetry and Blood Oxygenation
Pulse oximetry is a noninvasive method that uses light to test oxygen levels in the blood. Oxygen levels that are too low could be detrimental to your health. Blood oxygenation (SpO2) readings are used to monitor patients under many circumstances such as during procedures requiring anesthesia, lung medication dosing, increased activity scenarios, ventilator implementation, and sleep apnea diagnosis.
Pulse oximetry may also be used to check a person’s health if they have any heart or lung conditions. Normal blood oxygenation levels for an average adult range between 95% and 100%. Oftentimes, looking at blood oxygenation data over time provides more meaningful insights than from a single measurement. The FDA therefore suggests using pulse oximeters to monitor decreased oxygen level trends.
How do pulse oximeters work?
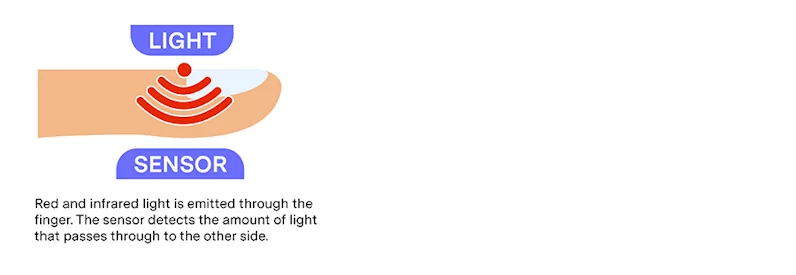
There are a few types of pulse oximeters available, with the most common options including fingertip, handheld, benchtop, phone-based, wearable, and multimodal oximeters. Typically, a pulse oximeter uses a clip or probe that attaches to a person’s finger or ear lobe. The probe emits red and infrared light from one side of the finger or earlobe and then detects the amount of light that passes through to the other side. Depending on the ratio of red and infrared light detected, the oximeter can then determine the amount of oxygen in the blood.
This method works due to how red light and infrared light are absorbed by oxygenated hemoglobin, or oxyhemoglobin (O2Hb), and deoxygenated hemoglobin, or deoxyhemoglobin (HHb). Oxyhemoglobin absorbs more infrared light than red light and deoxyhemoglobin absorbs more red light than infrared light. Other types of tissues do not absorb significant amounts of red or infrared light.
By comparing the amounts of red and infrared light detected by the sensor, the oximeter can determine an individual’s blood oxygenation level. Oxygenated blood has higher levels of oxyhemoglobin, explaining blood’s usual bright red color. More red light bounces back towards our eyes rather than being absorbed by the oxyhemoglobin. Blood with lower oxygen levels is a darker shade of red, due to higher levels of deoxyhemoglobin.
Categories of Pulse Oximeters
Pulse oximeters generally fall into two categories; prescription and over-the-counter:
Prescription Oximeters
Prescription oximeters are as the name implies and must be prescribed prior to use. The pulse oximeter must be reviewed and cleared by the FDA, undergoing clinical testing to confirm the accuracy falls within an acceptable range. These types of oximeters are normally used in hospitals and doctors’ offices, though some are prescribed for in-home use.
Over-the-Counter Oximeters
Over-the-counter (OTC) oximeters are sold directly to consumers. Unlike prescription oximeters, OTC oximeters may or may not be cleared by the FDA. These oximeters are instead used primarily for general wellness, sports, and aviation.
Limitations
Pulse oximetry isn’t a fool-proof science. Oximeters are most accurate within the 90% to 100% range, and least accurate when blood oxygen levels are below 80%. Most prescription oximeters’ accuracy is within 2% to 4% of actual blood oxygen levels. The accuracy of pulse oximeters decreases even further at lower oxygenation levels. For this reason, blood oxygenation values are more useful when looking at trends over time as opposed to a single reading.
There are additional factors that could influence the accuracy of readings. Specifically with fingertip oximeters, poor circulation, skin thickness, skin temperature, tobacco use, and fingernail polish may influence the accuracy of the pulse oximeter. Earlier reports regarding fingernail polish indicated that black, blue, and green polishes caused readings to be up to 10% lower than actual blood oxygenation values, with more recent studies determining that current fingernail polishes at most only lowered readings by less than 2%. There are also concerns regarding pulse oximeters’ accuracy between dark and light skin pigmentation. Current scientific evidence suggests that the variance in readings between dark and light pigmentation are typically small at saturations above 80%. The study, however, relied on previously collected health record data, meaning it did not correct for all the variables that could have influenced the reading. The FDA states that these findings need to be further evaluated to fully understand the relationship between skin pigmentation and oximeter accuracy.
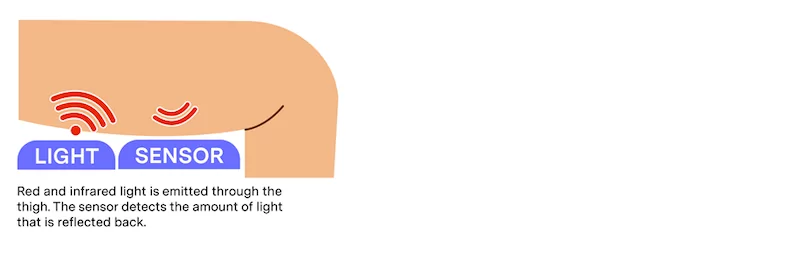
Pulse Oximetry in the Heart Seat™
The Heart Seat uses pulse oximeter technology that will be FDA-cleared to gather information on your body’s blood oxygenation. Called a photoplethysmogram (PPG), red and infrared light is emitted from the sensor through the thigh. Unlike a fingertip oximeter, instead of reading the amount of light that passes all the way through the tissue, the PPG sensor records the amount of light that is reflected back toward the sensor. By gathering information on oxygenation through every sit, valuable insights and trends can be formed and analyzed. With the Heart Seat, patients and doctors can monitor key clinical measurements through remote patient monitoring. Patients no longer need to remember to wear a smartwatch or put on a finger pulse oximeter. They can just sit on the Heart Seat without a second thought. With better adherence, patients can consistently track their health information. The seat will be an FDA-cleared device, initially requiring a prescription for use.

Interested in helping with research on the Heart Seat? Casana is currently looking for participants to help bring the future of in-home healthcare to a reality. You can sign up today for one of our clinical studies.
Disclaimer: All of the material provided above is for informational purposes only. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. Casana does not endorse any of the products or services mentioned in this post.
Recommended insights
New Data Advocates Shift to In-Home Healthcare, Casana Appoints VP of Research to Enhance Product Development
Exclusive data from internal Casana studies and new executive hire announcements.
Casana’s In-home Cardiovascular Monitoring Toilet Seat (The Heart Seat) Early User Experience Study
Interested in testing The Heart Seat from the comfort of your own home? Now’s your chance. Casana has launched our in-home research study formally titled “In-home cardiovascular monitoring toilet seat (The Heart Seat™) early user experience...Read More
Toilet Talk: The Heart Seat is Not Just Another Gadget
A Casana engineer on why working on The Heart Seat is an engineer’s dream.
