Hypertension and Comorbidities | A common and dangerous combination
Published: February 28, 2023
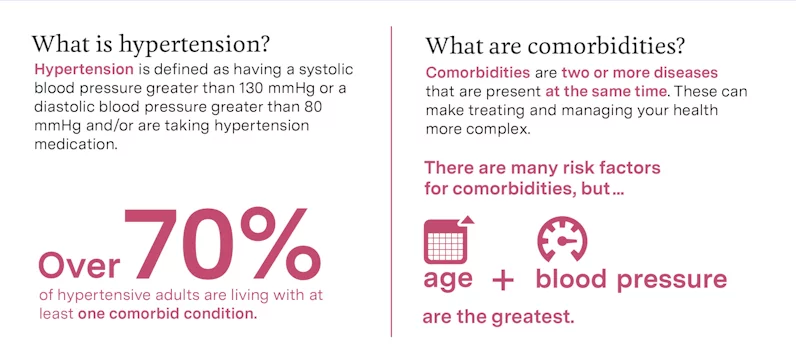
Having hypertension, along with other health conditions, can create a domino effect, increasing the likelihood of developing additional diseases over time. These additional health conditions are referred to as comorbidities. Over 70% of hypertensive adults are living with at least one other comorbid condition. Despite this increased risk of developing one or more comorbidities from hypertension, most hypertensive adults do not have their hypertension under control.
What are Comorbidities?
Comorbidities are two or more diseases that are present in a person at the same time.
While there are many risk factors for comorbidities, age and blood pressure are the two biggest factors. Hypertension greatly raises your chances of developing other types of health issues such as brain, heart, or kidney diseases. In fact, for hypertensive adults over 60 to 65 years old, the probability of developing at least one comorbid condition reaches over 50%.
Dealing with multiple diseases can make treating and managing your health increasingly complex. Understanding how each disease impacts your body may help you identify, manage, and prevent comorbidities.
Common Comorbidities
There are many comorbidities that are prevalent in hypertensive patients. Some of the most common comorbidities associated with hypertension are as follows:
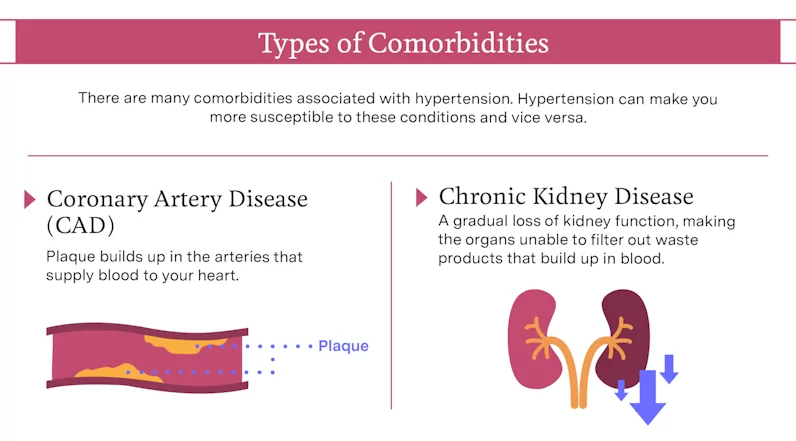
Coronary Artery Disease
Coronary artery disease (CAD) occurs when plaque—a combination of cholesterol, fatty deposits, and other substances from your diet—builds up in the arteries that supply blood to your heart. This buildup causes the vessels to narrow over time and can eventually lead to a blockage. Blood has more trouble flowing through the blood vessels when this happens and the oxygen supply to the heart’s muscle tissues can eventually become completely cut off. This event is called a myocardial infarction, more commonly known as a heart attack.
When someone has hypertension, their artery walls are under more stress due to high blood pressure. If left untreated, this extra force can cause damage to the arteries, making them more susceptible to plaque buildup and therefore at a higher risk for developing CAD.
In patients with CAD, their obstructed arteries can lead to a buildup of blood. As the fluid accumulates, so does pressure. If this becomes a chronic issue, the patient can also develop hypertension. Notably, studies have shown that decreasing systolic blood pressure by 10 mmHg and diastolic blood pressure by 5 mmHg in adults with CAD reduces the likelihood of having a cardiovascular event caused by the condition by 24%.
Chronic Kidney Disease
Your kidneys have a very important role in maintaining your health. When blood circulates throughout the human body, it collects excess fluid and waste products from the cells. Once the blood reaches the kidneys, the fluid and chemicals are then filtered out and expelled from the body in urine.
Chronic kidney disease (CKD) is a condition where there is a gradual loss of kidney function. Being unable to properly filter your blood poses a major threat to your health and can lead to a variety of possible complications, including hypertension. Without fully functioning kidneys, the excess fluid normally disposed of will begin to accumulate. As this process occurs, your blood volume increases. The more liquid traveling through your blood vessels, the more pressure there is being exerted onto the vessels, which will eventually lead to high blood pressure (or higher blood pressure). Your kidneys also produce hormones that regulate blood pressure, which are not released if the organs are damaged.
Hypertension impacts your kidneys in multiple ways that can result in CKD. Not only can high blood pressure harm the blood vessels that feed the kidneys and other organs, but it can also damage the kidneys’ nephrons, or little filters. In both of these cases, the kidneys’ filtration systems become compromised and are then unable to get rid of the waste products, as well as the excess fluids from the blood.
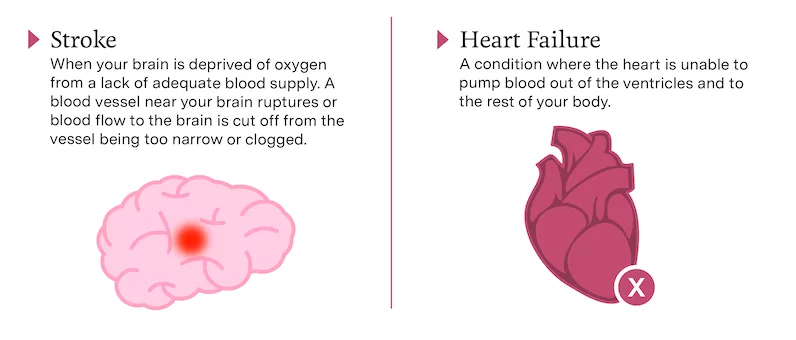
Stroke
A stroke occurs when your brain is deprived of oxygen from insufficient blood supply. There are two kinds of strokes, hemorrhagic and ischemic. A hemorrhagic stroke happens when a blood vessel near your brain ruptures and is unable to deliver the blood where it needs to go. This only accounts for about 13% of strokes. An ischemic stroke occurs when the blood flow to the brain is cut off from the vessel being too narrow or clogged. Ischemic strokes make up about 87% of strokes.
A study found that subjects with hypertension were over three times more likely to experience a stroke than those without. The occurrence of ischemic and hemorrhagic stroke can be largely prevented by controlling your blood pressure. Because of the added physical stress on their inner walls, hypertension is more likely to lead to ruptured or narrowed blood vessels. Therefore, maintaining normal blood pressure is crucial for lowering your risk of developing a stroke.
Heart Failure
Heart failure is a chronic condition in which your heart is unable to pump enough blood out of the ventricles and into the arteries, as well as to your other organs. Hypertension is a frequent cause of heart failure. When you have high blood pressure, your heart has to work harder to pump the blood against that pressure into your arteries. Over time, the added stress on the heart muscle will cause concentric hypertrophy to occur.
Concentric hypertrophy occurs when the walls of the heart chamber thicken, while the size of the chamber itself stays the same. While one may think this would make the heart stronger, having thicker walls actually makes the muscle more stiff and prevents it from being able to contract as easily. If the hypertension is left untreated, concentric hypertrophy can eventually give rise to eccentric hypertrophy, or a growth in the size of the heart’s chamber rather than its walls. Dilation of the ventricle damages the muscle tissue, weakens the ventricular walls, and ultimately makes your heart muscle unable to effectively pump out blood to circulate through your body.
On the other hand, heart failure can also cause hypertension. When the heart is unable to pump as much blood out of its left ventricle, it can cause a chronic backup of fluid throughout the pulmonary circuit or the blood vessels that transport blood between the heart and lungs. If left untreated, this will typically lead to pulmonary hypertension or high blood pressure within this circuit.
Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease or COPD is a chronic inflammatory lung disease that causes blocked
airflow from the lungs. Every person has a trachea, commonly known as a windpipe, that splits into two large tubes known as bronchi. One bronchus feeds your left lung with air while the other brings air into your right lung. In patients with COPD, their bronchi are constantly inflamed and coated in a thick layer of mucus. This causes their airways to narrow and restricts the amount of air that can be inhaled.
In addition to the bronchi, small arteries carrying blood from the heart to the lungs become more narrow from the inflammation. This means blood will travel much slower through the lungs and it leads to a buildup of pressure in those vessels. High blood pressure in these arteries is referred to as pulmonary hypertension.
Uncommon Comorbidities
It is important to point out that the less common comorbid conditions are frequently underestimated and treatment often consists of only self-prescribed medications. Rheumatic diseases and psychiatric diseases are two examples of uncommon comorbidities associated with hypertension that we shouldn’t ignore.
Rheumatic Diseases
Rheumatic diseases affect joints or tendons causing pain and inflammation. They are typically autoimmune diseases, which means that the body is being attacked by its own immune system. An example is rheumatoid arthritis (RA) where the body’s immune system attacks joints and results in pain, stiffness, and swelling.
More than 50% of premature deaths in RA are attributed to cardiovascular disease (CVD) from hypertension. Cardiovascular disease is an umbrella term for conditions involving the heart or blood vessels such as coronary artery disease, heart attack, and heart failure. Unfortunately, researchers still don’t know exactly how autoimmune diseases can cause hypertension. Researchers believe it may have to do with the relationship between the immune system and the kidneys. Because of this relationship, the inflammation from a dysfunctioning immune system can damage the kidneys, which can lead to hypertension.
Psychiatric Diseases
Although researchers have yet to find solid evidence to prove that psychological stress alone causes hypertension, psychiatric disorders like depression have been linked to the condition. There is a strong connection between blood pressure and psychology. When you are under stress, your body releases a wave of hormones. Some of these hormones act on your cardiovascular system and raise your blood pressure by increasing your heart rate and constricting your blood vessels. This is also known as our “fight or flight” response. Since acute anxiety or sadness can raise blood pressure, it makes sense that patients dealing with chronic anxiety or depression from a psychiatric disorder may be more likely to also develop chronic high blood pressure.
How to Manage Your Hypertension & Comorbidities Better on Your Own
Having both hypertension and additional comorbidities makes managing your health increasingly challenging. A recent study identified four major reasons why most people often have trouble managing their hypertension on their own.
1 | Stop viewing your hypertension and comorbidity as one illness
Researchers have found that those who have multiple conditions tend to look at their health as a single experience. In other words, they treat their conditions as a whole without paying much attention to the repercussions of each condition independent from the other. Doing so causes individuals to have more trouble separating their illnesses and thus keeping a close enough eye on each condition.

2 | Don’t leave your hypertension on the back burner
You may have heard hypertension be referred to as the ‘silent killer’ because it is very common for high blood pressure to be asymptomatic. As a result, the condition is repeatedly given lower priority than more “visible” comorbidities and it is often overlooked.

3 | Look for ways around conflicts between the conditions’ treatment plans
If the treatment plan for hypertension conflicts with the comorbidity’s treatment plan, the one for hypertension is generally neglected. For example, maintaining a diet that is both low-sodium and low-sugar, a diet suitable for hypertension and diabetes, is difficult to do because there aren’t many foods that can satisfy both of these requirements. Although finding solutions under circumstances like these can be challenging, it is important not to allow one treatment plan to limit the other as much as possible. It may be worth speaking with your doctor if you are having trouble dealing with conflicts between your treatment plans.
4 | Keep track of all of your medications
In addition to making positive changes to your daily behavior, hypertension usually needs to be treated with medication. If you are hypertensive with one or more comorbidities, you may need to take additional medications on a regular basis to maintain each condition. Keeping track of the time of day, dose, name, purpose, and frequency you need to take each medication can be very difficult. Consistently tracking medications is a major reason why patients struggle with keeping their hypertension under control. Fortunately, groups like the American Heart Association and the U.S. Department of Health & Human Services offer some free resources like this Medications Log and this Daily Medicine Schedule to help you manage your medications and overall health.
Recommended insights
What doctor’s want you to know about Hypertension Management
A conversation with Casana Co-Founder, Cardiologist Karl Schwarz, MD.
Cracking the Commitment Code: Understanding Why Blood Pressure Adherence Is So Difficult
Blood pressure management is a critical aspect of maintaining overall health and preventing cardiovascular diseases. However, despite the known benefits of adhering to blood pressure management routines, many individuals find it challenging to maintain consistent adherence...Read More
Casana and Cleveland Clinic Successfully Conclude Cardiac Rehab Stress Shifts Study
Casana, in collaboration with Cleveland Clinic, has concluded a pilot study called the Cardiac Rehab Stress Shifts Study. The study aimed to evaluate the performance of the Casana Heart Seat™ in measuring shifts in blood pressure...Read More
